Antibiotic resistance: what it is, how it manifests itself and how to fight it
Antibiotics have revolutionized the treatment of bacterial infectious diseases, but they must be used correctly. The 5 fundamental rules
{getToc} $title={Table of Contents}
What are antibiotics
It is a class of drugs, which begins somewhat from a chance discovery. Just think of the story of penicillin, identified in 1928. Alexander Fleming, in the laboratory, discovered a mold that had destroyed the surrounding bacteria. But only after a long time, in 1941, it was understood that what happened meant laying the basis for the discovery of a drug against bacterial infections.
It was penicillin, in fact, the substance that was capable of killing bacteria in mold. Fleming worked with Howard Florey who was then at Oxford University and then with Ernst Boris Chain, a Jewish biochemist who escaped from Germany just before the war. And for this intuition the three scholars were awarded the Nobel Prize in 1945. Since then, many antibiotics have followed one another and are still available to doctors, with a basic general characteristic. They are compounds that are obtained from living organisms or through laboratory synthesis processes. They can block the growth of bacteria, therefore having a bacteriostatic action, or rather have a bactericidal activity, therefore capable of killing the germs themselves.
What does broad-spectrum antibiotics mean?
Obviously, not all antibiotics are the same. And also for this reason the choice of drug must always be made by the doctor, given that it is necessary to combat bacterial infections that differ in both location and severity. In any case, there are antibiotics that can act against different bacterial families and are therefore considered broad-spectrum.
In particular, in this case, the drug in question can act on both Gram-positive and Gram-negative bacteria. The term is linked to the characteristic color of the microscope. In the case of much more "narrow" objectives of the drug, the spectrum of action is considered reduced. Finally, sometimes two antibiotics can be used to control a specific infection. However, the drugs must act on different mechanisms of the bacterium, to avoid an antagonistic action of the drugs themselves. In any case, infections can also see the association of different bacterial strains and this helps to explain why more than one antibiotic is used.
How antibiotics work
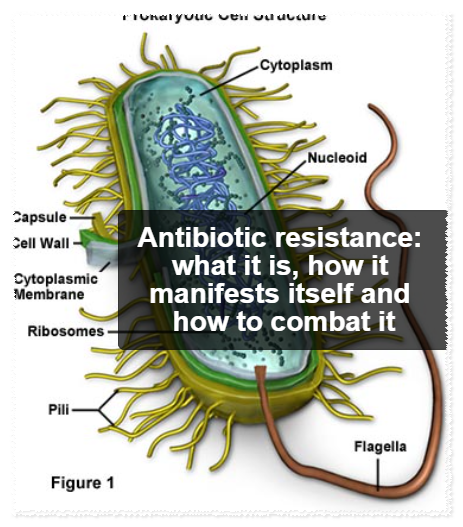
In addition to being chemically different from each other, the antibiotics that your doctor has available can also act differently. For example, those like amoxicillin inhibit the synthesis of the cell wall of bacteria, which therefore cannot develop normally. Cephalosporins, another family of drugs, also act on the same targets. Macrolides, another class of antibiotics, work by blocking the synthesis of proteins that are fundamental to sensitive germs. The same also happens for tetracyclines, which target the synthesis of proteins by bacteria.
Then there are quinolones which instead inhibit the replication of genetic material. Obviously these are only examples that help to understand the complexity of the situation.
Because we fear antibiotic resistance
Bacteria will become less and less sensitive to antibiotics. And so, after having been the protagonists of a miracle, they could now become less and less "miraculous" and progressively lose their power in treating these infections. A few years ago, the warning of Matthew Cooper and David Shales, authors of the book "Antibiotics: the perfect storm", sounded more or less like this. Unfortunately they were completely right.
Thanks to bad habits and the improper use of these drugs that have revolutionized the fight against infectious diseases, today finding antibiotics that are able to eliminate particularly "resistant" germs is increasingly difficult and this puts many people at risk who, perhaps due to pathologies or due to intrinsic weakness of the immune system, they can suffer the heaviest damage from the infections themselves. In Italy the situation is certainly not rosy. Antibiotic resistance leads to over 11 thousand victims per year. Unfortunately, the incorrect use of these drugs becomes the fuel for the worsening of this situation.
How do bacteria mutate?
Germs, of course, tend to change. And above all they reproduce at very high speed, which increases the risk of transformations of their characteristics. Consider that in optimal conditions some bacteria can double in number every twenty minutes. The antibiotic, especially if not used correctly, can trigger a series of natural survival mechanisms that the bacterium implements to escape the attack of the drug and to preserve the species.
What happen? Let's try to see some mechanisms. For example, the germ can "mix" some portions of its genetic material with that of another species, taking on its resistance characteristics. Sometimes, however, a bacteriophage is used, a sort of "transmission belt" that allows the germ to incorporate genes from another bacterium, or it can even happen that a fragment of DNA passes from one bacterial cell to another, modifying the invisible " attack points” of the antibiotic.
The result of all these steps is that the antibiotic, no longer finding the "handholds" necessary to kill the bacterium, becomes ineffective. It should also be remembered that the genes that favor resistance can overcome the "species" barrier of the host, so they are transmitted very easily even from one species to another and even in particular situations, such as for example in animal husbandry.
Who needs to be protected from antibiotic resistance
Bacteria are divided into two macro groups, Gram-positive and Gram-negative and differ in the thickness of the cell wall. Gram-negative bacteria, in addition to having a thicker cell wall, are made up of pathogens with a high capacity for adaptation and are the cause of the most common intra-abdominal infections, urinary tract infections, nosocomial or hospital-acquired pneumonia. Therefore, making the best use of antibiotics against bacteria of this type, and not only, appears to be of great importance. At the point where we are The goal is to protect everyone, obviously.
But let's remember that the people truly at risk are those with seriously debilitating illnesses, which greatly reduce the defenses against infections, especially if admitted to hospitals or assisted healthcare homes. As long as we are able to defend ourselves, these resistant, or partially resistant, microorganisms do not cause damage, even if they become part of our endogenous intestinal bacterial flora (which we wouldn't want anyway).
But if we are hospitalized, if we need treatments that reduce our immune defenses, major surgery or transplants, then resistant bacteria become such a risk as to call into question, in the not too distant future, the very possibility of continuing to perform these procedures that are so invasive, so modern but also so dangerous in some respects.
Don't use antibiotics for viral infections
The period is the one at risk. The first sore throats of the season arrive, perhaps accompanied by some signs of fever and fatigue. Here, in these circumstances, rely on the classic herbal tea, if you prefer milk and honey, if you prefer the regenerating power of chicken broth or the strength of the vitamins contained in citrus fruits and colored vegetables. If you really feel broken, ask for advice at the pharmacy to find some symptomatic ones that will help you fight the ailments.
But don't make the mistake of choosing an antibiotic independently, perhaps promising to finish the package that is still in the medicine cabinet. And not only because seasonal ailments, especially in this period, are linked to the action of the many circulating viruses and not bacteria (the antibiotic is completely useless and ineffective against viruses!). nor because it must always be the doctor who indicates not only whether it is necessary to use this fundamental drug, but which must not be abused, indicating times and methods of administration. The real reason that must push us to always refer to the doctor to assess whether the antibiotic is needed is another: we must all fight together the resistance that bacteria are developing towards these drugs, which is becoming a public health problem.
How to combat antibiotic resistance
Countermeasures to combat bacterial resistance to antibiotics involve everyone. Doctors and healthcare personnel are recommended, in accordance with WHO indications, to always follow the protocols for the prevention of infections, starting with hand washing and prescribing antibiotics only when necessary, in accordance with current guidelines . But a lot also depends on all of us. First of all, you must avoid "do it yourself" by taking an antibiotic left in the medicine cabinet when fever and sore throat appear. It is a serious mistake because these drugs have precise indications and are not all the same. Before taking an antibiotic, a doctor's prescription is always necessary because antibiotics are only useful against bacteria and are completely ineffective if the infection is viral in nature.
Then you need to follow the directions carefully. One of the most frequent mistakes, in the case of antibiotic therapy, is to stop the drug as soon as the symptoms disappear and perhaps the fever drops. The treatment must be continued for the entire period indicated by the doctor, otherwise there is a risk of not completely curing the infection and above all of making the drug less effective in the event of new attacks by the germs.
Five simple rules for using them well
- The antibiotic must be prescribed only by the doctor and not taken because it may have remained in the medicine cabinet.
- The treatment must be carried out for the entire period indicated and not only as long as the fever and discomfort remain.
- Interrupting treatment carries the risk that not all the microscopic enemies will be eliminated and that some of them will become resistant.
- Expired or already opened drugs due to a previous infection should be thrown away: not all drugs have the same indications and objectives.
- Antibiotics are active only on bacteria. Therefore they do nothing against viruses: they should not be used to fight the flu.
Bibliographic sources
Antibiotics: what they are, what they are for and how to use them, Mario Negri Pharmacological Research Institute (IRCSS)
European Day and World Antibiotic Week 2023, Istituto Superiore di Sanità
AIFA initiatives for the World Week on the conscious use of antibiotics, AIFA